Styloid-Carotid Artery Syndrome
From the Department of Otolaryngology- Head and Neck Surgery, Charles R. Drew University of Medicine (Dr. Avitia and Dr. Osborne), the Osborne Head and Neck Institute (Dr. Hamilton and Dr. Osborne), and the Head and Neck Cancer Center, Cedars-Sinai Medical Center (Dr. Osborne), Los Angeles.
Ear, Nose & Throat Journal· April 2006
A 42-year-old commercial pilot was placed on medical leave because of frequent episodes of syncope that occurred when he turned his head to the extreme right lateral position. The patient’s partner said that these syncopal episodes were accompanied by jerky movements that resembled seizure activity. The patient would regain consciousness as soon as his head became realigned in the midline. As his symptoms increased in severity and frequency, he began to experience transient episodes of blindness in his right eye.
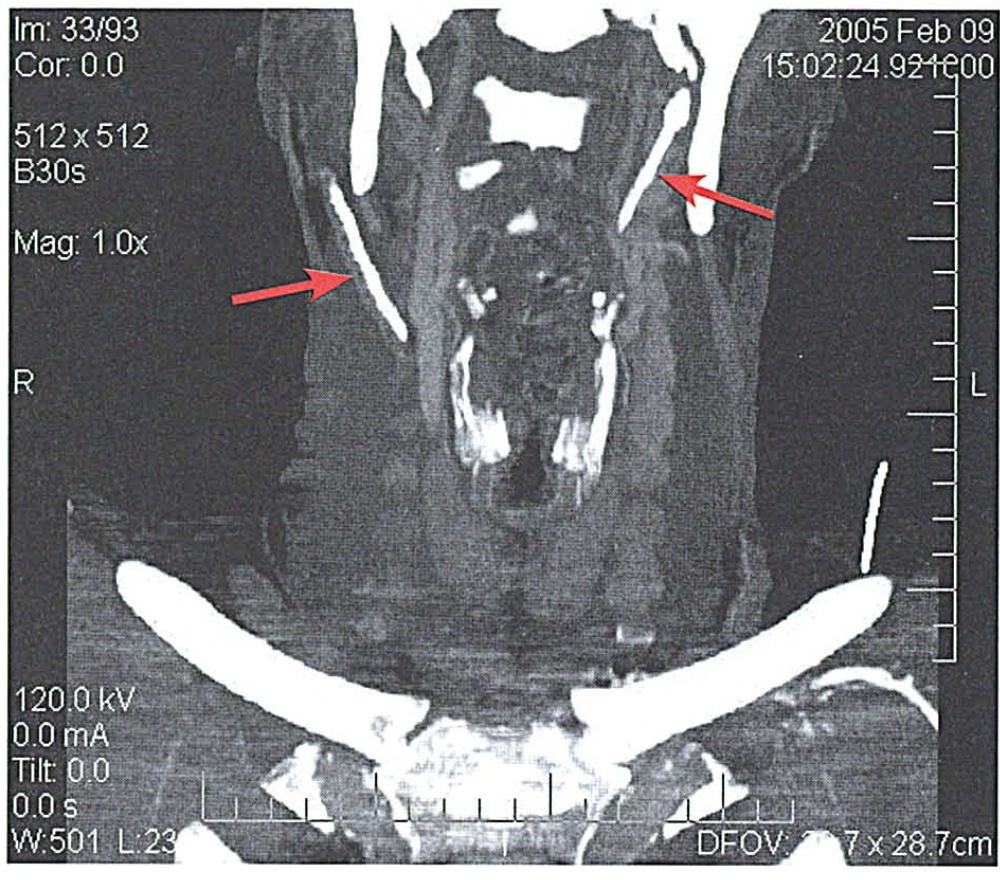
The patient was seen by a neurologist, who ordered computed tomography (CT) and magnetic resonance imaging (MRI) of the head and neck with contrast; the MRI demonstrated no abnormalities. Magnetic resonance arteriography and magnetic resonance venography showed that the circle of Willis was patent, as were the internal and externaljugular veins bilaterally. However, computed tomographic (CT) angiography demonstrated that the styloid processes were elongated and the stylohyoid ligaments were calcified bilaterally (figure 1). In addition, the lumen of the right carotid artery appeared to be narrowed by 50% as a result of its tortuous course around the calcified ligament.
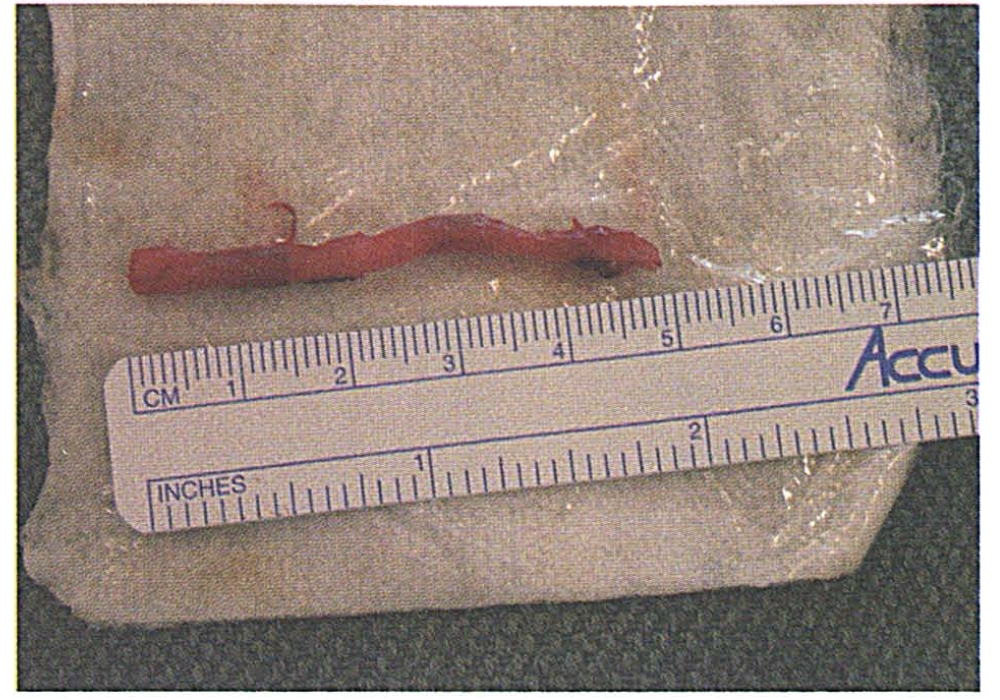
The patient was taken to the operating room for surgical resection. Intraoperative neurophysiologic monitoring detected no signs of abnormal brain activity. He successfully underwent a transcervical resection of approximately 5 em of the elongated right styloid process and calcified ligament without complication (figure 2). His postoperative course was uneventful, and his syncope resolved.
In 1937, Eagle and Durham described 2 cases of post-tonsillectomy pharyngeal pain that had been caused by an elongated styloid process; this condition is now known as Eagle’s syndrome. In 2002, Prasad et al described their experience with 58 cases of Eagle’ s syndrome over a 10-year period. “All of their patients had present ed with a chief complaint of pain, and their diagnosis was based on palpation of the tonsillar fossa, a panoramic x-ray, and a positive lidocaine infiltration test. All of these patients underwent resect ion via a transoral approach. The longest styloid process excised measured 3 em.
In 2000, Bafaqeeh subclassified Eagle’s syndrome into two types: its classic form and an entity he called styloid carotid artery syndrome. Our patient’s presentation, diagnosis, and treatment more closely resembled styloid carotid artery syndrome than classic Eagle’s syndrome. On presentation, his primary symptoms were syncope and associated neurologic manifestations, including blindness, that had been caused by not only an elongated styloid process but by a calcified stylohyoid ligament, as well. On axial CT, the extent of calcification of the stylohyoid ligament was not well appreciated, nor was its close association with the carotid artery. However, the association was clearly demonstrated on the sagittal reconstruction of the CT angiography. In view of the extent of the calcification and its proximity to the carotid artery, a transcervical approach was favored over the transoral approach.
Special recommendations for the diagnosis and management of patients with styloid-carotid artery syndrome include sagittal CT angiography with reconstruction when clinical suspicion is high, intraoperative neurophysiologic monitoring, and a transcervical approach to resection.
Sinusoidal vertical-axis rotation testing revealed normal gains and phase lags at four frequencies, a finding that is consistent with a peripheral vestibular disorder. A finding of abnormal symmetry toward the left at two frequencies was consistent with an incompletely compensated left peripheral vestibular disorder.
On laboratory evaluation, the complete blood count was normal, as were the lipid panel and thyroid-stimulating hormone level. A 5-hour glucose tolerance test demonstrated impaired glucose tolerance and abnormally elevated insulin levels.
Thin-section axial computed tomography of the temporal bones detected evidence of a demineralized cochlear capsule, such as is seen in patients with inner ear otosclerosis.
The patient was treated with a combination of risedronate 30 mg twice weekly, a calcium supplement with vitamin D, and a calcium supplement with fluoride to address the otic capsular findings. He was placed on a modified hypoglycemic diet to address the blood glucose and insulin findings.
The patient returned after 3 month s of treatment. He reported only two spells, which occurred on successive days after he had flown on five airplane flights. Both spells were brief and less severe. Neither the nausea nor the aural fullness on the left returned. Follow-up laboratory data showed a reduction in the serum insulin level, but not to a normal level. Repeat sinusoidal vertical-axis rotation testing elicited evidence of a shift in peripheral vestibular function indicating improvement, although some abnormal symmetry toward the left remained.
When evaluating patients with vestibular symptoms by electronystagmography, the usual expectation is that the source of the vestibular symptoms is hypoactive caloric functioning of the vestibular labyrinth. In the case described herein, the abnormality was reflected as a hyperactive response to the bithermal caloric stimulation in the left ear. The finding that the left ear was the source of the symptoms is consistent with the findings of aural fullness and reduced distortion-product otoacoustic emissions in the left ear.
Demineralization of the bony labyrinthine capsule, as occurs in some forms of otosclerosis, responded to the combination of the bisphosphonate, calcium, vitamin D, and fluoride. The patient’s change in diet achieved some success in reversing his hyperinsulinemia. The persistent elevation of the insulin level may explain the brief recurrence of symptoms on the 2 successive days after he had taken five airplane flights.
References
I. Eagle WW, Durham NC. Elongated styloid processes. Report of two cases. Arch Otolaryngol 1937;25:584-7.
2. Prasad KC, Kamath MP, Reddy KJ, et al. Elongated styloid process (Eagle’s syndrome): A clinical study. J Oral Maxillofac Surg 2002;60:171-5.
3. Bafaqeeh SA. Eagle syndrome: Classic and carotid artery types. J Otolaryngol 2000 ;29:88-94.